Gen Z is having less sex, so why are they getting more STIs?
Though we love to talk about sex, Gen Z aren’t so good at actually putting their money where their mouths are betwixt the sheets. But while our lust is low, the same can’t be said for our rates of STIs which have gone up by a quarter in the last year. Alice Wade speaks to Dr Malik to find out why we’re more infected, despite dry spell.
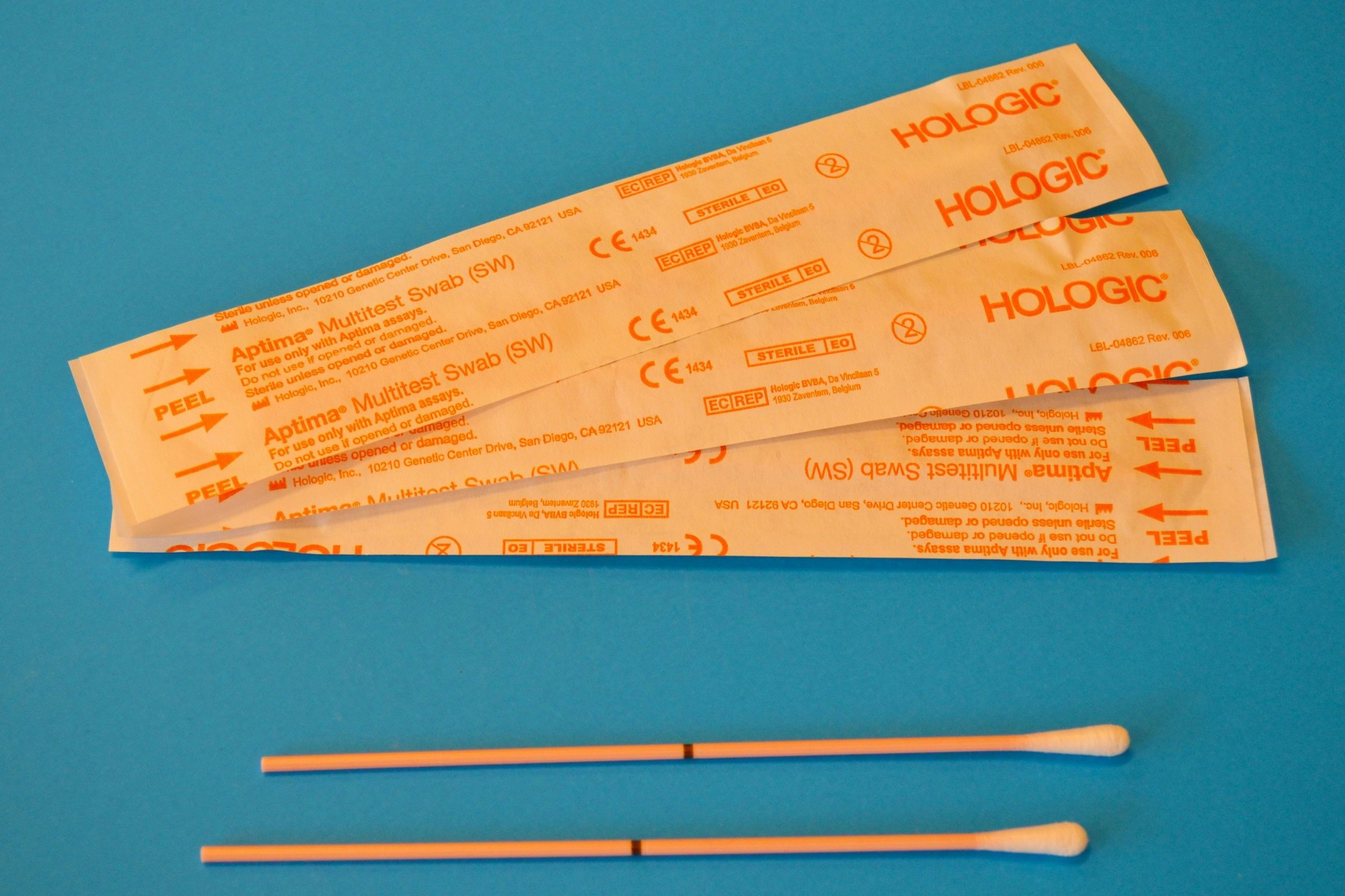
Credit: Unsplash, Testalize Me.
If you’re a Gen Zer, you’ve likely come across the data that shows that our generation is having much less sex than people our age 20 years ago.
According to the study, as many as one in four Gen Z adults – who as of 2024 can be as old as 27 – confess to never having sex, while the same number of women admit to not having had any sex in the last year.
There are a multitude of reasons for the decline. For one, we’re more anxious, jobless, and less likely to ever own property. A hornless cluster of sad snowflakes.
But one thing that we are in surprising abundance of is STIs.
According to the UK Health Security Agency, 392,453 people were diagnosed with an STI in 2022, which is 24% higher than the previous year.
So, when the research says people are having it off less, why are STIs having such a field day?
Dr Shazia Malik, a consultant OBGYN and UK medical director at Daye, says there are a few factors at play here.
Safe sex education / STI education
Though Gen Z has objectively had a hugely positive impact on sexual openness, broadening linguistic boundaries to cater to the vast array of sexual desires, preferences and kinks, Malik theorises that we might not be as knowledgeable about safe sex as we think.
“There may still be gaps in knowledge among Gen Z regarding STIs, their transmission, and the importance of regular testing,” she says.
“This lack of awareness can lead to risky behaviours and a false sense of security. There is widespread health misinformation on social media apps, and some of this misinformation has spread to STIs as well.”
STI risk awareness
Another theory is that Gen Z aren’t aware of the importance of safe sex because they don’t see the threat of contraction as very high.
Malik suggests: “Now that the HIV epidemic is largely in the past, the rates of public education on the importance of safe sex have fallen, which means Gen Z are not as aware of the importance of safe sex practices.”
Evidence suggests this isn’t just an issue for younger people as 53% of HIV diagnoses are now being given to people over 50, suggesting the lack of safety awareness is more widespread regardless of age.
And while it’s true that the number of people in the UK living with HIV is much lower than when it originated – thanks to awareness, better protections and PrEP – in the same year that diagnosis rates for STIs like chlamydia, gonorrhoea, and HPV increased, so too did diagnosis of HIV.
In fact, the rate of diagnosis for HIV went up 27% from 2020 to 2022, with 6% of that being between 2021 and 2022.
Though this might look alarming, it’s important to remember that the number of people living with HIV in the UK is around 95,900 people, a relatively low number.
If left untreated, HIV, or human immunodeficiency virus, can go on to cause the more serious and sinister, AIDS, or acquired immunodeficiency syndrome.
The current cause of action following an HIV diagnosis is to use antiretroviral therapy, which works by reducing the viral load of HIV in the blood, slowing down the progression of the virus and increasing an individual's life expectancy.
Read more: We need to talk about STIs and mental health
No sex during the pandemic
The spike between 2021 and 2022, may also be partly down to the pandemic, Malik explains.
“The pandemic and the reduction in regular screening during its duration played a significant role in the proliferation of STI infections.”
Since people weren’t really allowed out of their houses, there were far fewer opportunities for casual sex and for the spread of STIs.
Dating apps might be to blame too
Despite the lacklustre amount of sex being had, behavioural differences might have contributed to the rise.
As Malik explains, “The prevalence of social media and dating apps in modern dating culture can facilitate casual encounters and quick hookups, potentially increasing the likelihood of unprotected sex and higher STI transmission rates.”
“While the overall frequency of sexual activity among Gen Z may be lower than in previous generations, various societal and behavioural factors contribute to the rising rates of STIs within this demographic” she concludes.
Now we’ve looked at the reasons for STI inflation, here is Malik’s essential STI information guide.
Symptoms of STIs to look out for
No one likes a visitor from the invisible man. But that’s basically what happens when you’re infected with most STIs. “Just cute old, mostly symptomless chlamydia,” Jez from Peep Show famously said. He too, had the invisible man over.
“This is particularly true for women and assigned female at birth (AFAB) individuals,” Malik explains.
Though women are more likely to be negatively affected by STIs, they are actually less likely to have symptoms, making testing all the more important.
“Symptoms of an STI can vary depending on the infection but may include genital discharge, sores or ulcers on the genitals, pain during urination or sex, and abnormal vaginal bleeding.,’ Malik explains.
Risks of untreated STIs
Most STIs, including chlamydia, gonorrhoea, syphilis, and mycoplasma genitalium (M. gen) can have pretty disastrous effects if left to their own devices.
The effects vary according to the infection and how long it’s been left for but the worst case scenario could result in infertility and or permanent nerve damage.
And as Malik explains, the consequences don’t end there.
“For instance, gonorrhoea and syphilis can lead to serious health issues such as pelvic inflammatory disease, heart complications, memory problems, and nerve issues” she explains
The resulting pelvic infections can then lead to “chronic vaginal discharge, chronic pelvic pain and abnormal bleeding, such as heavy periods”.
“In addition, while not universally recognised as an STI, Bacterial Vaginosis (BV), can also impact fertility outcomes, as it has been shown to increase the patient's risk of miscarriage and preterm labour.”
If this is all starting to sound a little depressing, don’t forget that you’re chances of getting to this stage are drastically reduced if you are testing regularly!
How often should we test for STIs?
I’m sure by now, it comes as no surprise that the advice is basically to get tested pretty regularly. Malik suggests getting a new test every time you sleep with someone new.
“Since certain STIs can be symptomless and easily spread unknowingly, it is advisable for sexual partners to undergo testing before engaging in unprotected sex.”
“Testing frequency can vary but should be done at least annually or more frequently if engaging in high-risk behaviours or experiencing symptoms,” she adds
For example, gay or bisexual men are at higher risk so should be tested more frequently. Between three and six months if recommended. Further, sex workers and those who practise chemsex should also receive more frequent testing, along with those who’ve been diagnosed with TB or hepatitis.
Where to get tested for STIs
“Testing for STIs can be done at sexual health clinics, healthcare providers' offices, or through home testing kits, such as Daye's STI home screening kit” she says.
Daye’s new testing service offers users the chance to get a full picture of their sexual health, including screening for trichomoniasis and mycoplasma genitalium, as well as the standard chlamydia and gonorrhoea test. BV, thrush and other non sexually transmitted infections can also be tested for with the upgraded package.
If payment isn’t an option for you, most big cities around the UK offer free home screening services, providing an easy and discreet way to test. You don’t have to tell your mum or get in the stirrups, and the only time you leave the house is to deliver your unsuspecting package to a post box.
Free at home tests in London can be found here.